Israel Ranks Highest in COVID-19 Vaccination Rate
Per capita, Israel is inoculating its 9.2 million citizens faster than any other country.
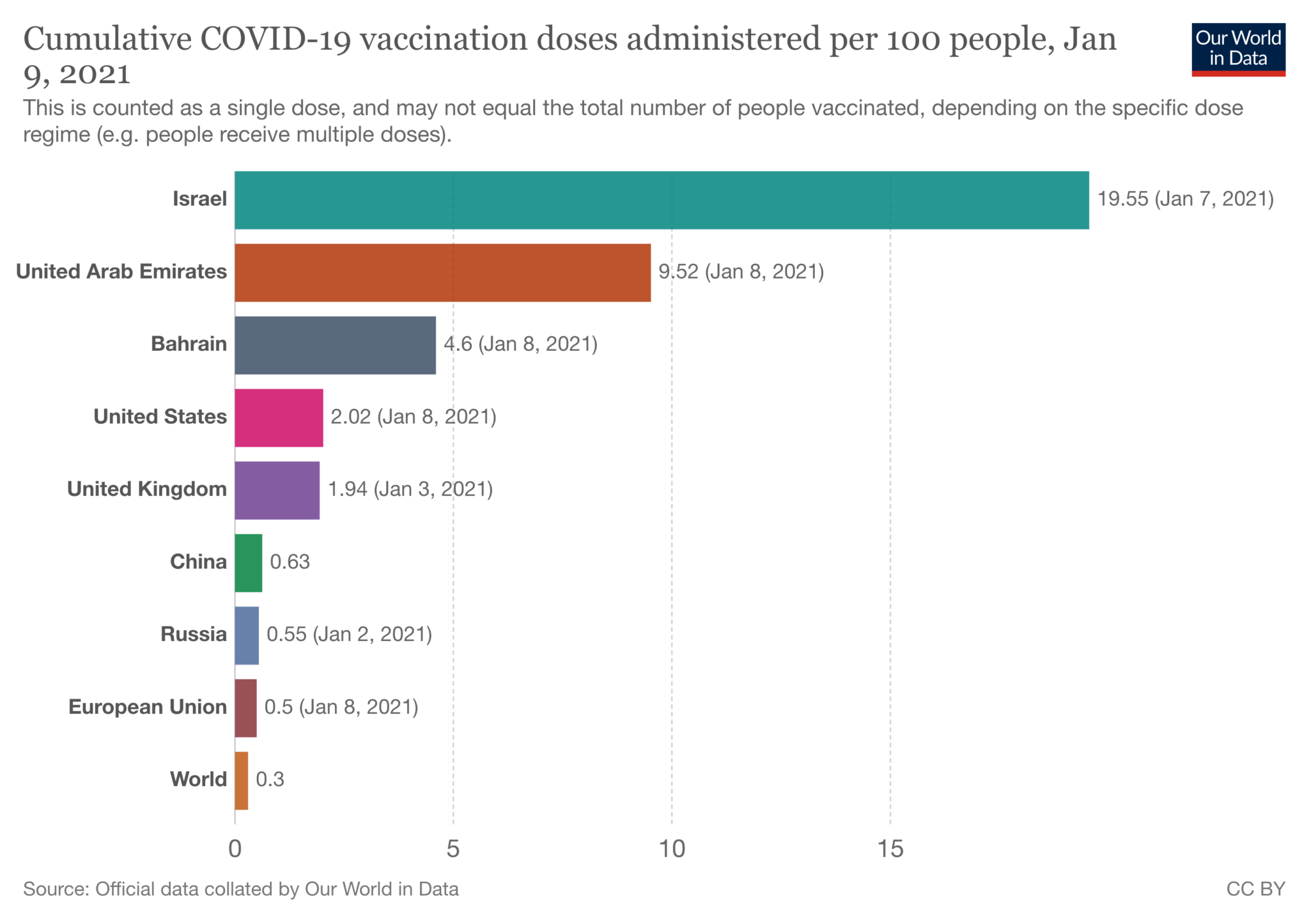
Worldwide, Israel is being heralded as the leader in getting its citizens vaccinated against COVID-19. Per capita, the country beats every other nation, hands down, in vaccinating millions of Israelis in the first few weeks of the vaccine’s availability there, according to the Our World in Data online publication.
Israeli media reports that the country is seen as a test case for the vaccine manufacturers because if it works to beat the virus there, other nations will be eager to buy the life-saving antidote to a pandemic that has killed millions around the world and crushed economies everywhere.
As of Jan. 9, about 2 million Israelis had been vaccinated against COVID-19, amounting to some 16 percent of its population. The country is vaccinating 150,000 people every day – including Shabbat – and Prime Minister Benjamin Netanyahu has called for daily vaccinations of 175,000 by mid-January. Netanyahu was the first Israeli to be vaccinated Dec. 19.
Certainly, the population size of the country helps. Israel’s 9.2 million citizens are even less than Georgia’s 10.6 million, let alone the U.S. population of 331 million. But, according to Atlanta Dr. Harry Heiman, Israel’s successful vaccination program is primarily due to its universal healthcare system. Moreover, “Israel knows what it means to put policy in place at a national level and roll it out,” said Heiman, clinical associate professor in the Department of Health Policy & Behavioral Sciences in the School of Public Health at Georgia State University.
According to Israel’s 1995 National Health Insurance Law, the country’s entire population is entitled to comprehensive health coverage, ensuring that no citizen could be denied coverage on the basis of lack of funds. Each person chooses to become a member of one of four kupat cholim, or sick funds. In American terms, these are government funded health maintenance organizations, or HMOs.
Each of the four Israeli healthcare providers – Clalit, Maccabi, Leumit and Meuhedet – are required to provide a standard basket of medical services. Citizens pay a health tax of about 5 percent of their income to help pay for the costs. Based on each kupat cholim’s share of the population, it receives a per capita payment from the government to cover those costs.
According to David Chinitz, professor of health policy management in the School of Public Health of the Hebrew University-Hadassah Faculty of Medicine, “The health plans contract for service provision from physicians, hospitals and other providers in a manner similar to U.S. managed care plans, especially HMOs.” Writing in Tablet magazine, Chinitz also noted that citizens may move their membership between plans every year without limitation.
“While the percentage of the population switching health plans is low (between 1 percent and 2 percent per year), the health plans work hard to keep their members and attract new ones,” Chinitz said. He added that the competition is only over quality of service because Israel’s health indicators, such as life expectancy and infant mortality, are among the best in the world.
Heiman believes that the United States’ national leadership failed, relying on the states that did not have the leadership nor the resources to put their vaccination plans into effect. “Georgia, like all states, had to put together a vaccination plan in October,” which allowed reasonable planning time, Heiman said. “But it doesn’t appear much happened between putting it on paper and administering the plan.”
When asked if he had read the plan, Heiman responded that he had read the “first, second and third versions.”

The plan, he said, calls for vaccinating under existing infrastructures such as pharmacies and providers. Pharmacies such as Walgreens and CVS were to vaccinate the priority populations in elderly institutions, but they don’t have the staff.
Until the last COVID relief legislation passed by Congress at the end of 2020, the states weren’t given adequate resources to vaccinate their populations, Heiman said. Yet, that should not have totally affected Georgia’s response to the vaccination demand, he added. “Georgia has a rainy-day fund for emergencies and economic downturns, and I can’t imagine a more appropriate use of that fund” than for the vaccination roll-out.
“My hope is that the incoming Biden administration, based on the team I’ve seen, will be more responsive and we will have more consistent messaging coming from the federal government.”
He also hopes that the Centers for Disease Control and Prevention in Atlanta will be “allowed to do its job, which has been difficult,” adding that “it will take a long time to regain its reputation and public trust.”
Biden’s nominee to head the CDC is Rochelle Walensky, currently the chief of infectious diseases at Massachusetts General Hospital and professor of medicine at Harvard Medical School. According to Biden’s announcement of her nomination, Walensky, who is Jewish, is a leading expert on virus testing and treatment and has been on the frontlines of Massachusetts’ pandemic response.
While Israel continues its vaccination program, it is also experiencing high daily COVID new case numbers, despite the country being locked down a third time due to the pandemic.




comments