Breast Cancer Basics: First in a Series Do I Really Need That Mammogram?
Screening for breast cancer regularly is beneficial for your health, according to Dr. Barry Roseman.
Now that it is safer to venture out of our homes, you are probably wondering whether to go out and get that yearly mammogram that may be due or perhaps overdue. You may be wondering: Is it really necessary? And every year? Oy! And by the way, is that the only test I need, to stay out of trouble?
As it turns out, breast cancer screening with mammography is a really good idea. Besides being free (for most) it is extremely effective at finding early breast cancers. The premise goes like this: breast cancer is a progressive disease, so earlier detection will result in a lower stage of breast cancer at the time of diagnosis. Identifying breast cancer at an earlier, rather than later stage, is the main benefit of screening. The early detection/better outcome premise has held up through multiple clinical trials; in other words, there is a lot of science to back it up.
For screening purposes, we can define advanced stage cancers as those that are stage II or greater at diagnosis. With modern treatment, there is no difference in survival between early stage breast cancers (stage 0-I) and the population without breast cancer. Mortality starts to increase at stage II. In other words, if we are able to identify breast cancer before it reaches stage II, III, or IV, survival rates increase markedly. Mammograms help us do that.
Survival, of course, is not the only endpoint. Cost is important as well. To the extent that treatment is simpler, economic costs are less with early stage tumors. But more importantly, the earlier the diagnosis and treatment, the less suffering. Women with advanced breast cancers experience terrible pain and suffering from extensive surgery, cytotoxic chemotherapy, and post-surgical radiation. All of this is usually unnecessary in women with early breast cancers.
Like many, you might be concerned about the possible harms of X-rays, and whether those harms balance the benefits of mammography. FYI, people in the U.S. are typically exposed to about 10 times as much radiation as that from a mammogram every year, just from being outside in the sun. Thus, a mammogram is relatively risk-free when it comes to radiation exposure.
The benefits of screening are seen in every age group. From age 40 until at least age 75, breast cancer screening saves lives. Some age groups benefit more than others, but everybody benefits. There is remarkable unanimity of opinion as to the benefits of screening and its low risk.
And what about COVID-19? Is it possible to be exposed during the visit and exam?
I can only speak from my own experience, but our clinic and all of the hospital mammography units I have visited since Georgia “reopened” are being extremely careful with regard to screening, patient distancing and hygiene. Of course you should wear a face mask throughout the visit, and insist that all of the staff and other patients are wearing masks!
So the answer to the first questions is: YES! You really need that mammogram, if you want to find a breast cancer early enough that it is simple to treat with minimal pain and morbidity and will not likely affect your lifespan.
Is that all I have to worry about? Is a yearly mammogram enough?
For those at average or below average risk of developing breast cancer during your life, as long as you keep getting your annual mammograms you should be fine. If there is an abnormality that turns out to be cancer, it will likely be a small, easily treatable tumor.
But what if you are higher risk for developing breast cancer or have been told you have “dense breasts”? You may need to be watched more closely and more frequently, and you might benefit from other types of imaging.
How would you know if you are at higher than normal risk?
Your risk of breast cancer increases with age, but there are other factors – mostly out of your control – that may increase your risk. While this is somewhat of an oversimplification, here are some examples of various risk categories:
Extremely high risk: Hereditary breast cancer syndrome (BRCA1 or BRCA2 mutation)
High risk: Mother, sister or daughter with breast cancer, or atypical cells on a breast biopsy
Above average risk: Other relatives with breast cancer, increased breast density (see below)
Average risk: Women without any family history or other known factors
Below average risk: Not everyone can be average or above average!
What is breast density?
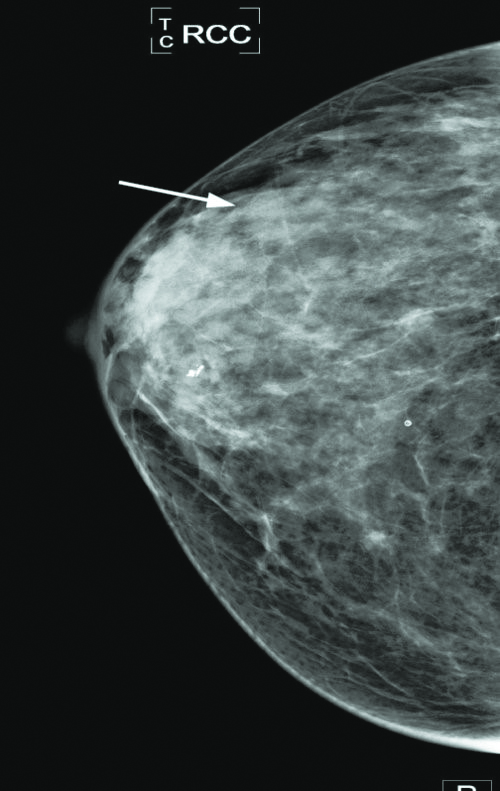
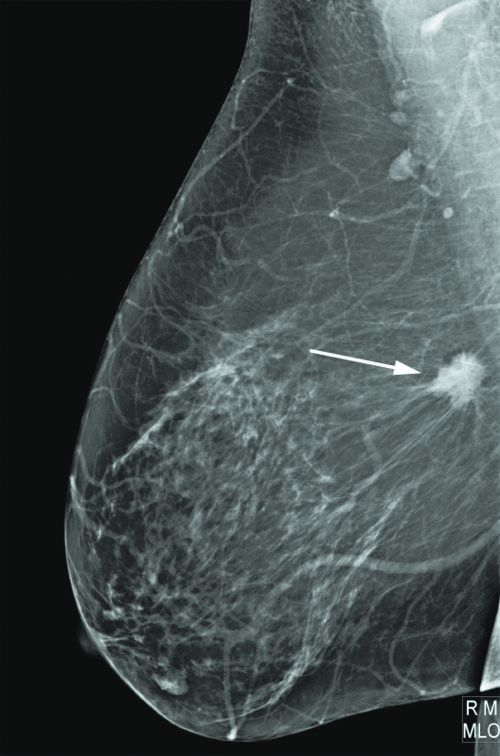
On a mammogram, density is simply the degree of active breast tissue seen, and it is graded by the radiologist as A, B, C or D. Women with category C or D density (heterogeneously dense or extremely dense) are considered “dense.”
I equate breast density with overly active or “busy” breast tissue, probably your breasts’ natural response to your own estrogen since puberty. Interestingly, increased breast density tends to be inherited.
So why is breast density a problem?
There are two reasons:
First, breast density makes breast cancers harder to find during screening.
Second, patients with increased breast density actually have an increased risk of developing breast cancer.
For women with dense breasts (category C or D) we often recommend additional imaging, since the mammogram is harder to read and subtle changes could be missed. In fact, all women with D density (extremely dense breasts) need supplemental imaging because the mammogram is nearly impossible to read as “normal” – since it is so hard to see through all of the tissue!
It also turns out that women with dense breasts are more likely to develop “missed” or “interval” breast cancers, those which pop up as symptomatic cancers between annual mammograms. As such, they are usually more advanced stage cancers with a worse prognosis.
What if I need additional screening?
If you are higher than average risk, or have dense breasts, we generally recommend additional screening beyond your yearly mammogram. Since mammograms are not perfect, instead of simply doing more frequent mammograms it makes sense to use other breast imaging modalities, especially those that can find breast cancers that mammograms cannot see.
This is the first of a series of short articles about breast cancer that I hope is informative. I will discuss how we approach additional imaging for screening and diagnosis in my next article. If you have questions or wish to contact me, please call or email me, and I will be happy to respond.
Dr. Barry Roseman is a Breast Surgeon who owns Advanced Breast Care/ Surgical Oncology of North Georgia, Inc.,
www.advanced-breastcare.com. He can be reached at barry.roseman@gmail.com or
404-841-6262




comments